Is a Keto Diet Really Necessary to Enable Healing of Insulin Resistance, the Main Cause of Type-2 Diabetes?
A ketogenic or keto diet is a diet that is very low in carbohydrates, high in saturated fats and has adequate protein and fibre, that is meant to induce ketosis, i.e. switch most of the body into the alternate metabolic pathway of buring fat derived ketone bodies, instead of the usual glucose metabolism. It is prescribed for people in the early stages of type-2 diabetes, and is also popularly called as the low carb, high fat (LCHF) diet. This ‘food as medicine’ approach is reported to work better than the usual drug regimen of insulin and metformin1.
However, the keto diet is a radically different diet to the traditional diets that most people are used to. It is understandable to cut off the addictively tasty high sugar (sucrose), high glycemic index/high glycemic load foods like sweets, white rice, and the many tasty food stuffs made from refined wheat flour (a.k.a maida). But, the keto diet goes well beyond this and requires cutting out even ‘healthy’ carbs like brown rice, whole wheat, lentils and even millets. The only lentils allowed are sprouted green gram and sprouted chickpeas, due to the fact that the process of germination reduces the carbs. The other banned items are all the starchy vegetables that grow below ground: potatoes, carrots, etc. and also all fruits! This is a tall order.
Given these stringent requirements, and the approximately 3× higher expense2 of the keto diet, the question arises:
Is it really necessary to go that far? Won’t just cutting out the tasty high glycemic index foods and excercising more regularly suffice?
To answer this, one needs to have a reasonably accurate model of how the body regulates blood glucose, and the breakdown of this regulation in type-2 diabetes.

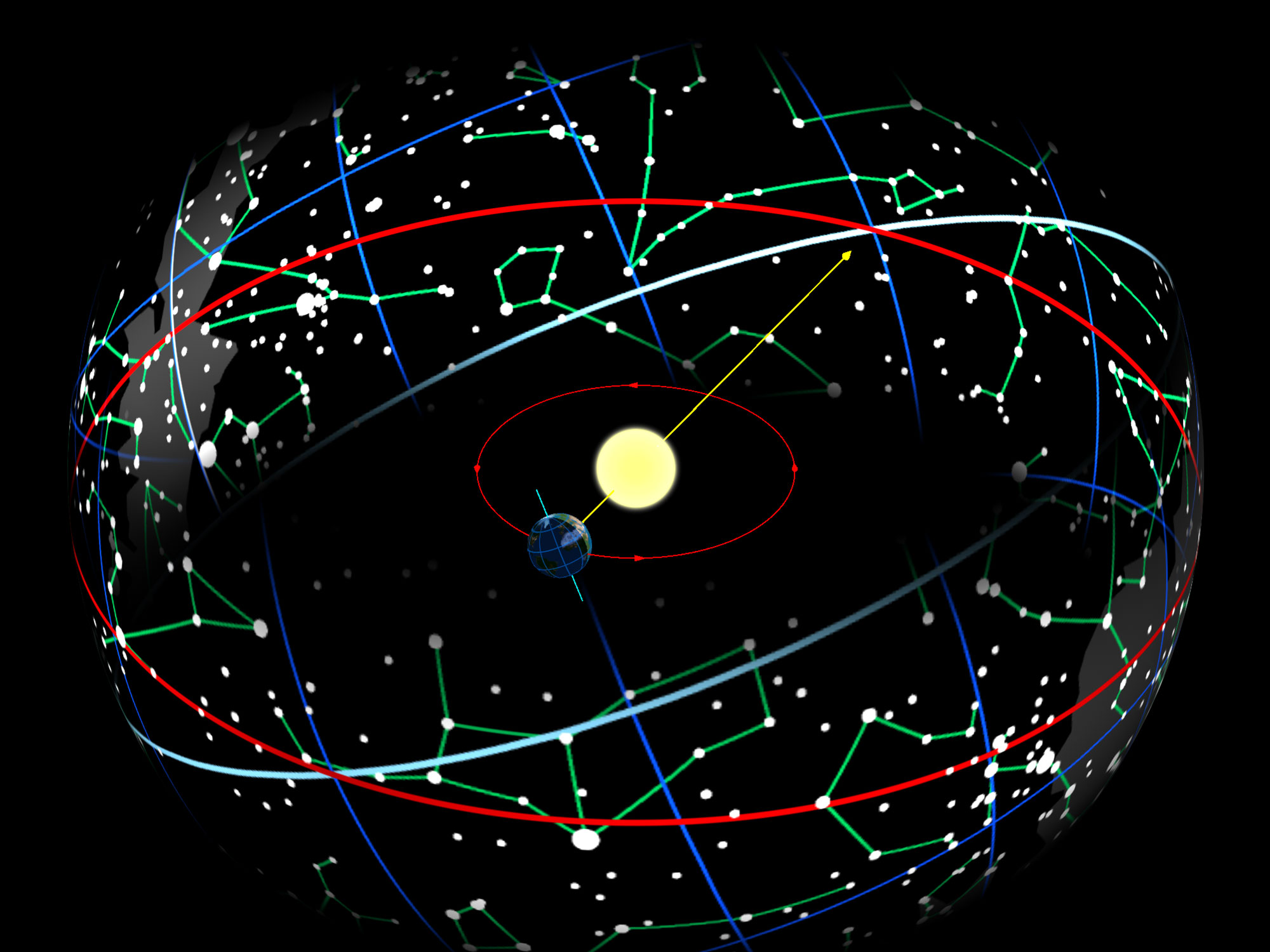
Figure 1: Some of the main players in blood glucose regulation. Note how everything that is digested in the intestines first proceeds to the liver via the portal vein. Source: Wikipedia: Portal Vein

Figure 2: Skeletal muscle and fat tissues, the other main players in blood glucose regulation. Source.
The main players are the following:
- the digestive system
- muscles
- fat tissue
- liver
- pancreas
Ordinarily, the digestive system is the main source of glucose. The muscles and fat tissue can act as both sources and sinks of glucose.
The liver is a versatile converter organ that can convert:
- glucose to glycogen (compact glucose polymer) and vice versa,
- proteins into glucose (gluconeogenesis),
- saturated fats into their storage form triglycerides, and triglycerides back into glucose and fats, and,
- saturated fats into ketone bodies.
The pancreas is the controller or director. The control is applied via two opposite acting hormones: insulin and glucagon.
The pancreas senses the blood glucose concentration (BGC), and attempts to maintain this in a range of about 80-140 mg/dL (dL = 0.1L = 100mL). Approximately, if BGC goes above 140, insulin secretion is increased, and this insulin signals the liver, muscles and fat tissue to take up blood glucose and thus lower BGC.
On the other side, if BGC falls below about 80, usually after a few hours of fasting, insulin is reduced and glucagon secretion is increased and this signals the liver, muscles and fat tissue to release glucose. After the glycogen stores are depleted, usually after about 32 hours, the liver ramps up gluconeogenesis to produce glucose and it also produces ketone bodies which become the main source of fuel for all tissues expect (mainly) the brain.
In type-2 diabetes (T2D) this happily balanced situation breaks down in a couple of ways:
- Over several years of gluttony and sloth, the muscles and fat tissues become resistant to responding to the insulin signal. Initially, the pancreas responds by increasing insulin secretion. But, a vicious spiral sets in. In parallel with the increasing doses of sugar needed to create the same level of pleasurable sensation, increasing production of insulin leads to increased insulin resistance and larger and larger doses of insulin are required to persuade these tissues to take up the same amount of blood glucose.
- After several cycles of this fruitless increased insulin production and increased insulin resistance, the pancreas’ insulin producing cells get fatigued and insulin production drops.
When these two happen, usually in succession, the body loses its ability to control blood sugar and the symptoms of hyperglycemia (BCG > 200) and later T2D result.
Given the above mechanism for T2D, the suggestion arises: what if carbs are cut out from the diet? Won’t this lead to lower insulin production and over some time help to bring the sensitivity of muscle and fat cells to insulin back to their previous levels?
This is exactly the key idea behind the keto diet as a therapy to help heal T2D.
At this point we have most of the information needed to answer the question posed: is such a radical diet absolutely necessary?
First, let us see what happens when no carbs are eaten3:

Figure 3: Rate of glucose production by gluconeogenesis in the absence of dietary carbs. Source: Fuel Metabolism in starvation–Cahill-2006
A small amount of glucose is still needed by the body, about 5 gm/hr, mostly by the brain. As a sanity check, note that 5 gm/hr of glucose = 5*4 kcal/hr = 23.24 Watts4, which corresponds to the often quoted fact that the brain, while only 2% of body weight, consumes 20% of the total energy expenditure of about 100 Watts (2000 kcal/day). In the absence of carbs in the diet, this amount is produced via gluconeogenesis from stored and dietary protein and stored, not dietary, fat in the form of triglycerides. All of this glucose production is regulated mostly by glucagon. Only low to very low amounts of insulin are needed to modulate any BGC peaks produced by gluconeogenesis in excess of requirements. Such low levels of glucose production and associated low need for insulin production is what will maximize the chances for the body’s insulin resistance to heal.
At this point, it is worth mentioning the case of run away ketosis, which leads to the life threatening condition of keto acidosis. Ketosis, the production of ketone bodies from fats is usually well regulated by the joint action of glucagon and insulin. Glucagon acts like the accelerator pedal, while insulin as the brake pedal. High glucagon levels gets the process started, and even the lowered levels of insulin secretion in T2D is usually sufficient to regulate it and keep it from going out of control and causing keto acidosis. In type-1 diabetics, there is almost no insulin production and these people are at the highest risk to keto acidosis, and so a keto diet is not recommended for type-1 diabetics.

Figure 4: Table 1 from Beyond weight loss: a review of the therapeutic uses of ketogenic diets1. Note the concentrations of insulin and ketone bodies (KBs) during normal regulated ketosis in column 3 vs. unregulated keto acidosis in column 4.
Next, let us see what happens when some “good” carbs are ingested by someone with T2D:

Figure 5: Carbs in Brown Rice. Source: Google/USDA
A typical serving of brown rice (1 rice cup ≈ 3/4 cup, 1 cup = 236.6 ml) contains about 109 gms of carbs and assuming it takes about 4 hours to be completely absorbed, can potentially provide 27 gm/hr, which is way above the fasting glucose production and consumption of 5 gm/hr in a keto regime. This extra glucose inflow from the large surface area of the intestines results in a BGC spike, which then requires turning off glucagon and turning insulin production back on to bring it down. Also, most of the body’s tissues will switch back from burning ketones to glucose. While this can bring down BGC, it also leads to increased production of ghrelin which causes a hunger for carbs, which if acted on, switches off ketosis completely. All this results again in hyperglycemia due the insulin resistance in T2D.
So, yes completely cutting out carbs is a necessary purgatory to allow insulin resistance to heal. In a well planned keto/LCHF diet, the only source of carbs comes from the (above ground) vegetables. These are necessary to provide a source of fibre to maintain a healthy gut bacteria culture and to also provide indispensible micronutrients. The total amount of carbs from typical servings of these vegetables is very low, about 20–30 gm/day. Assuming they are spread out in 2 meals, each meal provides about 15g and further assuming a 3 hr absorption period, the glucose provided is about 5 g/hr. So, for a 6 hour period gluconeogenesis can be switched off, providing some rest to the liver. Of course, the liver is still busy converting the saturated fats into ketone bodies.

Figure 6: Don’t be fooled by appearances: Purgatory in not a piece of cake. Going through keto purgatory or a carb holiday is necessary to restore insulin sensitivity.
Usually, a keto diet takes about 3–6 months to help the body’s insulin sensitivity to heal. After this healing, it becomes possible to reintroduce healthy carbs, i.e., the non-addictive low glycemic index and low glycemic-load carbs.
Regular exercise, is the most effective way to improve and maintain insulin sensitivity of muscles and fat tissues. Excercise and sticking to healthy carbs are required to prevent falling back into the vicious cycle of insulin resistance and T2D.

Figure 7: Source: The essential role of exercise in the management of type 2 diabetes.
Footnotes:
Paoli, A., Rubini, A., Volek, J. et al. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr 67, 789–796 (2013). https://doi.org/10.1038/ejcn.2013.116 , https://www.nature.com/articles/ejcn2013116
As a typical example: rice provides 56.7 kcal/₹ vs. butter’s 12.6 kcal/₹. This is calculated based on current (May-2025) market prices for white rice and unsalted butter. Rice: ₹63.15/kg, 358 kcal/100gm; Butter: ₹570/kg, 717 kcal/100gm.
Cahill GF Jr. Fuel metabolism in starvation. Annu Rev Nutr. 2006;26:1-22. doi: 10.1146/annurev.nutr.26.061505.111258. PMID: 16848698. https://doi.org/10.1146/annurev.nutr.26.061505.111258 , https://pubmed.ncbi.nlm.nih.gov/16848698/
A food calorie, which is capitalised as Calorie = 1000 calories or 1 kcal. A calorie is a physical unit, originally it was the amount of heat energy required to raise the temperature of water at 20°C by 1°C. James Prescott Joule in his famous series of experiments establishing the equivalence of mechanical work and heat measured that 4.184 units of mechanical work (Joules) equals 1 calorie. A Watt is an energy expenditure of 1 Joule/sec, it is a unit of power.